Shoulder joint replacement is a safe, effective procedure to help with painful conditions of the shoulder that cannot be adequately managed with medications or therapy.
Why are shoulder replacement procedures performed?
Your shoulder is a ball-and-socket joint that’s comprised of three bones: the upper arm bone (humerus), shoulder blade (scapula), and collarbone (clavicle). The ball, or head, of your upper arm fits into a shallow socket in your shoulder blade. When your shoulder is functioning properly, a thin, smooth tissue called synovial membrane makes fluid that lubricates the cartilage, allowing your shoulder to move smoothly and easily without much friction. The muscles and tendons that surround the shoulder provide support, and all these structures working together allow the shoulder to rotate through a greater range of motion than any other joint in the body.
Conditions such as arthritis can cause joints to lose their cartilage covering, and when you move, bone will move on bone without adequate protection. The result can be very painful, and you may experience a limited range of motion that hampers your ability to accomplish your daily activities.
What are the different types of shoulder replacement procedures?
Shoulder replacement surgery replaces the ball and sometimes the socket with man-made parts. Often the ball is replaced with metal and the socket is replaced with plastic. The components can be held in place with cement, or they can be made of material that lets new bone grow into the joint component over time, holding it in place.
There are several types of shoulder replacement surgery:
Hemiarthroplasty – the ball part of the head is replaced with an artificial joint that has a stem to extend into the shaft part of the bone. It’s usually used for fractures but is also often used for shoulders affected by arthritis.
Shoulder resurfacing – a different type of hemiarthroplasty that requires the removal of less bone. Instead of removing the ball part of the joint, a metal cap is simply placed over it.
Total arthroplasty – this replaces both the ball and socket and is usually used for specific types of arthritis. Your doctor will take into consideration your age, how badly worn the natural joint is, and the condition of the tendons around the joint. A total arthroplasty will sometimes be performed using a resurfacing component.
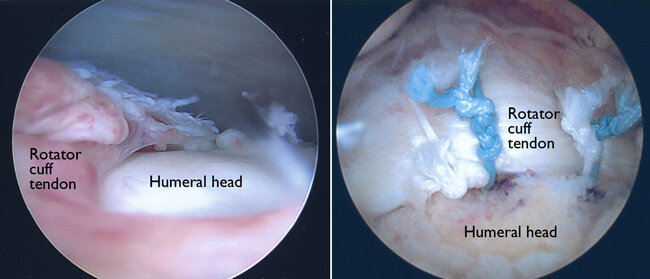
Reverse shoulder arthroplasty – artificial components are fitted in reverse, with the socket to the upper arm bone and the ball to the shoulder blade. It’s usually only performed on patients with severe arthritis and extremely poor rotator cuff tendons around the joint. It’s sometimes be used if a patient has both a severe joint fracture and poor tendon function.
I, as your surgeon, will determine the location, type, and extent of your shoulder problem before recommending the type of joint replacement that would be most suitable in your particular case.
Are you a candidate for shoulder replacement surgery?
The decision to have shoulder replacement surgery should be made in cooperation with you, your family, your family doctor, and your orthopedic surgeon